Most educational materials on pressure ulcer prevention tell you that the most common areas for pressure ulcers are under boney prominences such as the sacrum, ischium, and heels. However, an area that is frequently under-emphasized in pressure ulcer prevention education is skin breakdown under medical devices. Tissue damage under medical devices is therefore frequently overlooked when performing skin assessments, and this can result in devastating consequences of deep Stage IV pressure ulcers, adding to the burdens of pain, rehabilitation time, and costs of care.
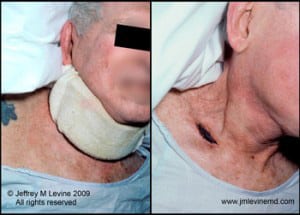 In my medical practice, for example, I cared for the patient in this illustration. He was 81 years old and suffered from neck pain related to osteoarthritis. He was frail, suffering from mild dementia, and lived at home with his elderly wife with a part-time home attendant. His primary care physician prescribed a soft cervical collar to be worn during the day. Unfortunately neither he nor his caregivers were instructed to remove the device periodically to check for potential skin damage. When he presented to the hospital for weight loss and poor oral intake, on removal of his collar an area of skin over his right clavicle was necrotic. Because this was an eschar and the base of the wound could not be visualized, the wound was staged as unstageable.
In my medical practice, for example, I cared for the patient in this illustration. He was 81 years old and suffered from neck pain related to osteoarthritis. He was frail, suffering from mild dementia, and lived at home with his elderly wife with a part-time home attendant. His primary care physician prescribed a soft cervical collar to be worn during the day. Unfortunately neither he nor his caregivers were instructed to remove the device periodically to check for potential skin damage. When he presented to the hospital for weight loss and poor oral intake, on removal of his collar an area of skin over his right clavicle was necrotic. Because this was an eschar and the base of the wound could not be visualized, the wound was staged as unstageable.
This area under a soft cervical collar is just one example of the myriad possibilities where ulcers can form under medical devices. Face masks and oxygen tubing in critically ill patients are frequently sources of skin breakdown. Immobilizing splints and other orthopedic devices are also major offenders in creating areas of skin breakdown. I have even seen skin breakdown under soft wrist restraints and abdominal binders placed to protect feeding tubes from being pulled out.
 A patient does not need to qualify as “at-risk” using a pressure ulcer prevention scale to necessitate skin-checks under medical devices. Although items on the at-risk scales such as nutrition, hydration, mobility level, etc. are important to quantify, areas under medical devices are always high-risk because they are localized areas of constant high pressure. The following table contains areas to consider as causing high risk for skin breakdown.
A patient does not need to qualify as “at-risk” using a pressure ulcer prevention scale to necessitate skin-checks under medical devices. Although items on the at-risk scales such as nutrition, hydration, mobility level, etc. are important to quantify, areas under medical devices are always high-risk because they are localized areas of constant high pressure. The following table contains areas to consider as causing high risk for skin breakdown.
The remedy for preventing skin breakdown under medical devices is device removal with inspection of the skin under adequate light. This should be done frequently – for hospitalized patients I recommend minimum every eight hours. Early skin breakdown is heralded by erythema, which when non-blanchable is called a Stage I pressure ulcer. This can be difficult to detect in dark skinned persons, and should be augmented with palpation for warmth and induration (firmness). Skin inspection under medical devices should always be emphasized on rounds with nurses, family members, and students.
* * * * * * * * * * * * * * * *
To access all blog posts on pressure ulcers and wound care click here.
